Inflammatory Bowel Disease Test Panel
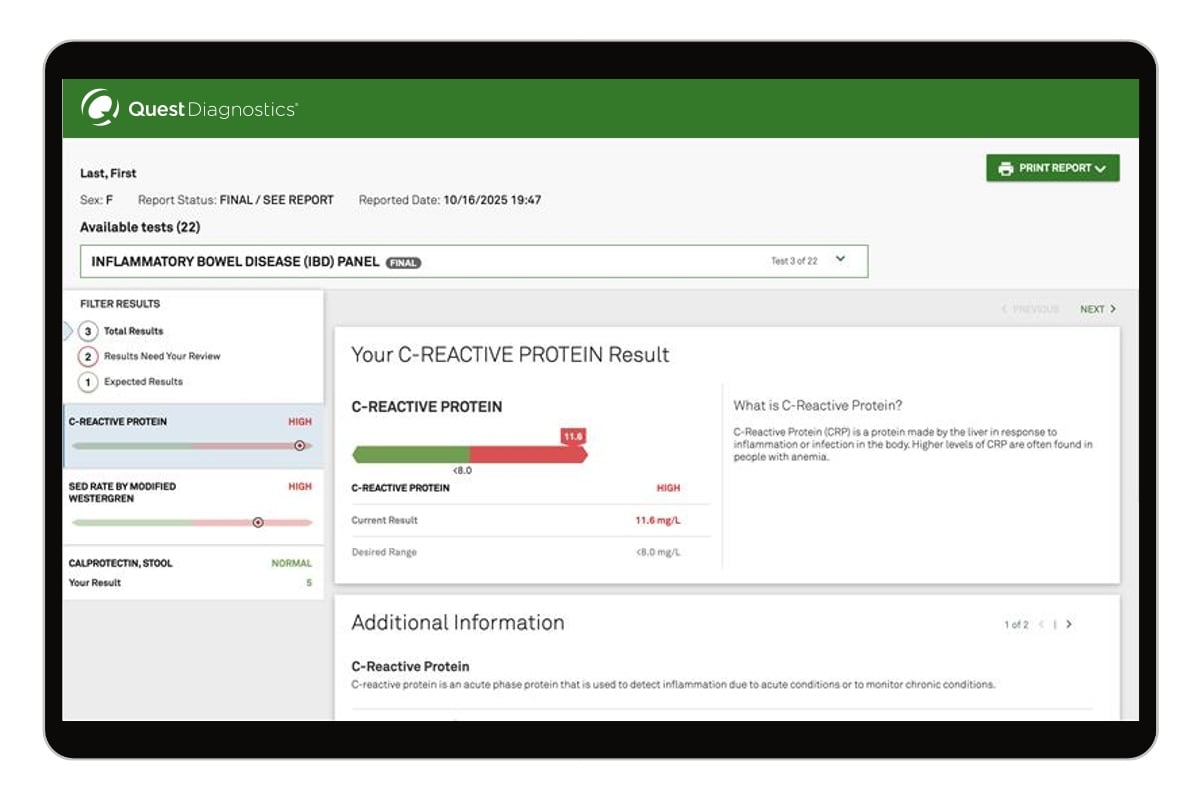
This test measures 3 key markers related to inflammatory bowel disease (IBD) in blood and stool – calprotectin, c-reactive protein (CRP), and erythrocyte sedimentation rate (ESR). Levels of these inflammation markers are associated with inflammatory conditions including ulcerative colitis and Crohn’s disease and may help you and your healthcare provider understand whether your symptoms could be related to these conditions or monitor your IBD and assess treatment response over time. Read moreThis IBD panel measures 3 key markers of inflammation – c-reactive protein (CRP), erythrocyte sedimentation rate by modified Westergren (ESR), and calprotectin – that may provide insight into intestinal inflammation often associated with inflammatory bowel disease (IBD).
Inflammatory bowel disease (IBD) refers to chronic inflammation of the intestinal tract. According to the CDC,1 an estimated 2.4 to 3.1 million adults in the United States live with some form of IBD. The condition occurs when the immune system mistakenly attacks healthy intestinal cells, leading to inflammation that can damage the digestive tract and often requires ongoing treatment. The two main types of IBD are Crohn’s disease and ulcerative colitis.
Measuring these inflammation markers can help you and your healthcare provider understand whether inflammation may be contributing to your digestive symptoms or help you track your inflammation levels and treatment response if you’ve been diagnosed with IBD.
Two markers of this test are measured in your blood (CRP and ESR), and calprotectin is measured in your stool. Both a stool and a blood sample are required for testing. You’ll need to book two appointments: one to pick up your stool sample container, and another to return it once you’ve collected your sample, and have your blood drawn. Blood will not be drawn at your first (container pickup) appointment.
No doctor’s visit needed. Buy this inflammatory bowel disease test panel online and visit a nearby Quest location.
While progress has been made in IBD research, researchers do not yet know the cause of this disease. Research shows that many things work together to cause IBD, including inherited genes and environmental factors.4 For example, cigarette smoking is an environmental factor that is known to increase the risk of Crohn’s disease. Researchers believe that once an IBD patient's immune system is "turned on," it does not know how to properly "turn off" at the right time. As a result, inflammation damages the intestine and causes symptoms of IBD.
No, but certain foods and liquids may cause your symptoms to get worse after you consume them. Every person’s body reacts differently, but food and drink that may make your IBD worse include the following:
- Beverages with alcohol
- Caffeinated or carbonated drinks
- Greasy food
- Food made with milk or dairy products
- Food high in fiber
- CDC Inflammatory bowel disease (IBD). IBD Facts and Stats. Accessed October 29, 2025. https://www.cdc.gov/inflammatory-bowel-disease/php/facts-stats/index.html
- CDC Inflammatory bowel disease (IBD). Inflammatory Bowel Diesase (IBD) Basics. Accessed October 29, 2025. https://www.cdc.gov/inflammatory-bowel-disease/about/index.html#:~:text=Inflammatory%20bowel%20disease%20(IBD)%20refers,symptoms%20and%20lead%20active%20lives.
- CDC Inflammatory bowel disease (IBD). Testing and Diagnosis for Inflammatory Bowel Diesase (IBD). Accessed October 29, 2025. https://www.cdc.gov/inflammatory-bowel-disease/testing/index.html
- Cleveland Clinic. Inflammatory Bowel Disease (IBD). Accessed October 29, 2025. https://my.clevelandclinic.org/health/diseases/15587-inflammatory-bowel-disease
- Cleveland Clinic. Understanding the Differences Between IBD and IBS. Accessed October 29, 2025. https://health.clevelandclinic.org/ibd-vs-ibs
- AGA Clinical Practice Guideline on the Role of Biomarkers for the Management of Crohn’s Disease. Ananthakrishnan, Ashwin N. et al. Gastroenterology, Volume 165, Issue 6, 1367 - 1399
- AGA Clinical Practice Guideline on the Role of Biomarkers for the Management of Ulcerative Colitis. Singh, Siddharth et al. Gastroenterology, Volume 164, Issue 3, 344 - 372